
Can we avoid the Genetic Ammiocentesis?
Genetic Amniocentesis is a prenatal diagnostic technique aimed at obtaining fetal karyotype. The karyotype is the number of chromosomes that are endowed with all people. Normal people we have 46 chromosomes distributed in 23 pairs (22 pairs of chromosomes called autosomes and 1 pair of sex chromosomes, XX or XY, which determine the sex of the fetus). Down syndrome or trisomy 21 is the most common chromosomal abnormality in new born infants; in this case, the individual has 47 chromosomes, and the alteration is that there are 3 21 chromosomes rather than two.
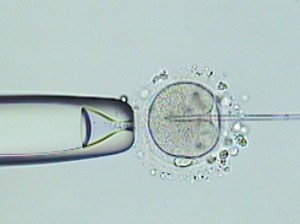
Is performed by inserting a needle through the mother’s abdomen and uterus and into the amniotic cavity where the fetus is surrounded by amniotic fluid. It is extracted by suction from 15 to 20 cc of the liquid. This test is usually performed between the 16th and 18th weeks of gestation. It is next to the Corionic biopsy, which we discussed in a previous post, what we know as “invasive tests” of prenatal diagnosis.
Amniocentesis is not a completely risk-free trial, although the frequency of complications is low. It is estimated that the risk of abortion or fetal loss after this procedure is 1% (ie, 100 women will undergo a test have an abortion). Other possible complications include premature rupture of membranes and Rh isoimmunization.
In most cases, genetic amniocentesis is done to rule out that the fetus is affected by Down syndrome. Traditionally, the most common indication for amniocentesis was “the age of the mother.” Since the 30s, it is known that the risk of Down syndrome increases as does the maternal age; that is why until recently, conducting a genetic amniocentesis is recommended for women over age 35. But using maternal age as a criterion for the performance of this test has several drawbacks: first, if we perform this test only to women over 35, we only diagnose 30% of fetuses with Down syndrome. On the other hand, the group of pregnant women over age 35 has increased in recent years (in 1980 accounted for 4.5% and 14% in 2007), in many cases have had trouble conceiving and do not want to take the risks inherent in amniocentesis.
That is why, in the last 20 years, have appeared different test called “screening tests or screening for chromosomal
 abnormalities” that are defined as those tests performed to identify, among the general population of apparently healthy pregnant women, those with higher risk that the fetus is a carrier of a chromosomal problem. There are not diagnostic tests as such, but allows the selection of pregnant women with risk of chromosomal abnormality and to which is indicated to carry a genetic amniocentesis (which is what will establish the definitive diagnosis).
abnormalities” that are defined as those tests performed to identify, among the general population of apparently healthy pregnant women, those with higher risk that the fetus is a carrier of a chromosomal problem. There are not diagnostic tests as such, but allows the selection of pregnant women with risk of chromosomal abnormality and to which is indicated to carry a genetic amniocentesis (which is what will establish the definitive diagnosis).
In recent years it is being used the so-called “first trimester combined screening.” Using a computer program that integrates maternal age, some values ??of two hormones in the mother’s blood and ultrasound measurement of fetal nuchal translucency combine with gestational age; the theoretical risk of Down syndrome is estimated. Determination of β-hCG and PAPP-A placental hormones in maternal blood is usually performed between week’s 9th and 12th and nuchal translucency (which is the measure of a cluster of transient liquid in the region of the fetal neck) and the extent of the fetus is between 11th and 13th weeks. By convention, when the risk is greater than 1/270 performing genetic amniocentesis is recommended. Through the combined first trimester screening we can detect about 80-90% of fetuses with Down syndrome.
Recently, articles have appeared in the scientific literature referring to the diagnosis of Down syndrome by studying the free fetal DNA in maternal blood. These new non-invasive diagnostic techniques (since they only require the completion of a blood test on the mother), although promising, are still under investigation and are not applied in clinical practice.
In summary, since genetic amniocentesis is a diagnostic technique that involves certain risks to pregnancy, you should only perform it on those pregnant women whose fetus present a high risk of chromosomal or chromosomal abnormality.
Dra. Ana Palacios, gynecologist at Instituto Bernabeu.
