Choosing a fertilisation technique when oocyte counts are poor. IVF or ICSI?
A low ovarian response is an increasingly common situation for clinicians. It is mainly associated with delayed motherhood and, accordingly, with lower ovarian reserves. In this type of patients, the number of oocytes retrieved after puncture is normally limited. In this situation, choosing the most adequate fertilisation technique, conventional IVF or Intracytoplasmic Sperm Injection (ICSI), may stir a little controversy (of course, provided that the sperm quality and the medical history lead us to consider conventional IVF as a reasonable option).
One could speculate about the possibility that ICSI improved the results in this group of patients insofar as it might contribute to reducing the chances of low fertilisation rates or even of not any oocyte being fertilised by conventional IVF.
Nevertheless, analysis of the data readily shows that the reality is otherwise and there are certainly no differences between both techniques as far as the chances of a total fertilisation failure occurring in these patients are concerned. Furthermore, fertilisation rates remain practically the same regardless of the technique used, and a similar number of embryos are collected.
Finally, no differences are found either in the most relevant clinical parameters, such as positive ?-HCG, clinical pregnancy and implantation rates.
Therefore, use of ICSI does not seem to have any positive effects on success rates when compared with conventional IVF in patients with a low oocyte count. For this reason, our opinion is that indiscriminate use of ICSI is not justified, especially in view of the unnecessary manipulation that gametes would have to experience.
Why do clinicians and embryologists sometimes change ART instructions from IVF to ICSI on the day scheduled for ovarian puncture and oocyte insemination?
One of the situations that embryologists commonly face on the scheduled insemination day is an abnormal sperm sample count and/or abnormal motility. This means that we have to change the planned treatment from IVF to ICSI. It is important to keep in mind that, in order to perform conventional IVF, sperm samples necessarily have to meet suitable count and motility parameters. If not, the following day, we could potentially find ourselves faced with a case of fertilisation failure or a fertilisation rate that is lower than expected and desired.
Retrieved oocytes could also turn out to be poor quality. In cases such as these, ICSI is advised in order to guarantee the best possible fertilisation rate.
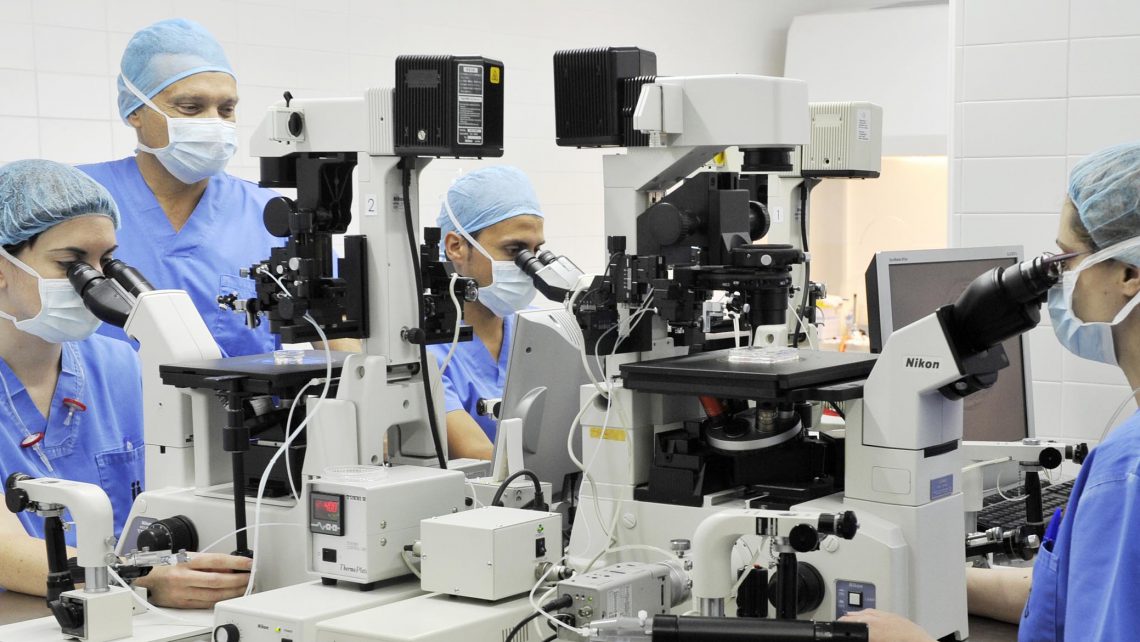
Whatever the circumstances, in their work and decision-making processes, our team of doctors and embryologists always strives to give couples the best possible outcome and achieve a successful conclusion to the treatment.
Jaime Guerrero, biologist at Instituto Bernabeu.
IT MAY ALSO BE OF INTEREST TO YOU:
