Ectopic pregnancy
Índice
What is an ectopic pregnancy?
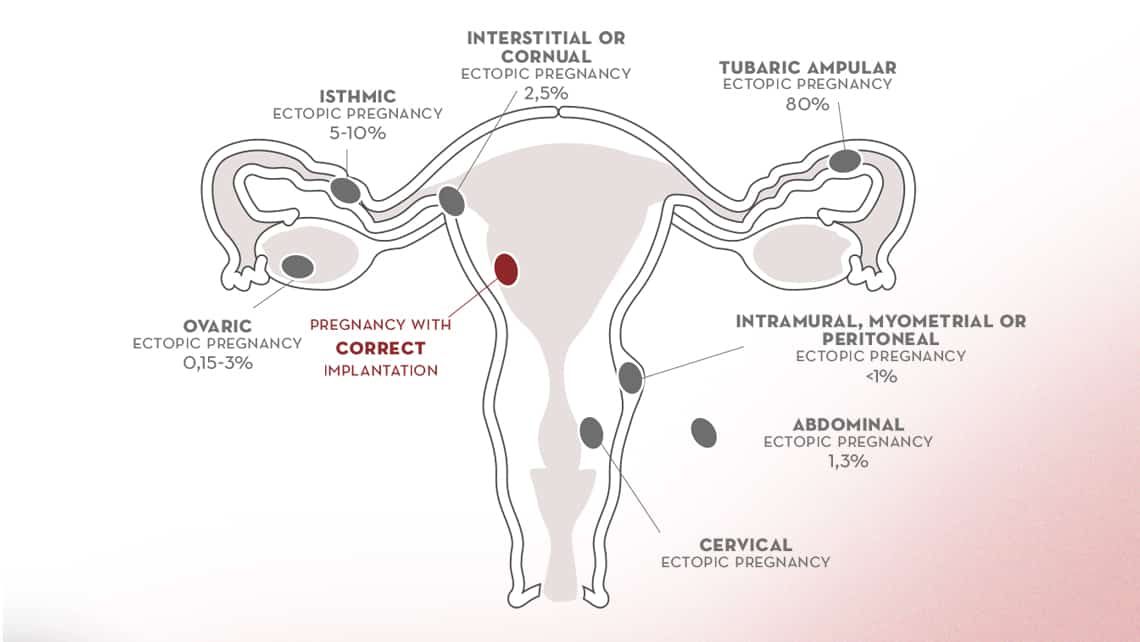
Any pregnancy implanted outside the endometrial cavity is called an ectopic pregnancy. It is a condition that occurs in 1-2% of all pregnancies. Despite the progress in its treatment and early diagnosis, its appearance and possible complications could compromise woman’s health and her reproductive future.
Types of ectopic pregnancies
Under normal circumstances, fertilization and embryonic development until its implantation occurs in the Fallopian tube. Abnormally, this process may occur towards the peritoneal cavity or in places close to the endometrial cavity.
- Tubal Ectopic Pregnancy: Sometimes, instead of moving towards the uterine cavity, the embryo stays where the fertilization took place causing a pregnancy in the fallopian tube. Tubal ectopic pregnancy is the most common type of ectopic pregnancies, accounting for 90% of them.
- However, if the embryo migrates abnormally towards the endometrial cavity, it can implant in the area of the union of the uterus and the tube: Interstitial or Cornual Ectopic Pregnancy.
- An embryo may implant abnormally in the myometrium, which is the area surrounding the cavity, causing myometrial ectopic pregnancy.
- Abnormal implantation may also occur in a caesarean or uterine scar caused by other circumstances.
- It can also be implanted in the cervical canal causing cervical ectopic pregnancy.
- Similarly, if the movement of the embryo occurs towards the interior of the peritoneal cavity, it can result in an ovarian ectopic pregnancy, being the second most frequent type with about 3% rate.
- In addition, implantation throughout the whole abdominal cavity has also been reported, both in the abdominal wall and the liver or spleen, which is called abdominal ectopic pregnancy.
Finally, although extremely rare, a heterotopic pregnancy has been described. This type of pregnancy occurs when there is normal embryo implantation within the endometrial cavity and another implantation in an ectopic form. Although this type of pregnancy is more frequent after assisted reproductive treatment, some cases have also been reported upon a spontaneous gestation.
Symptoms of ectopic pregnancy
Ectopic pregnancy may be asymptomatic, although it often causes vaginal bleeding in its first weeks. It can range from heavy to very light bleeding. Likewise, the abdominal pain is not very relevant and is not usually different from the pain that can be experienced in the first trimester of a normal pregnancy.
Therefore, an ectopic pregnancy can go totally unnoticed or can cause very mild symptoms that are often confused with a normal on-going pregnancy until the complication appears. The problem arises when the cells of the embryo invade the tissues where they have implanted, reaching significant blood vessels.
Similarly, when we are dealing with a developing tubal ectopic pregnancy it will end with a tubal miscarriage. Depending on the calibre of the affected blood vessel and the exact place where the embryo implanted, this type of pregnancy can cause abdominal pain with hardly any haemoperitoneum (blood in the peritoneal cavity) or, on the contrary, can become a very serious situation in which a blood vessel does not stop bleeding and can endanger the woman’s life if an adequate action is not taken immediately.
Sometimes, abdominal pain is not the most important symptom, but rather a pain that may appear in the right shoulder due to the activity of the nerves irritated by the pregnancy rupture.
Causes and risk factors of ectopic pregnancy
The most characteristic risk factor for an ectopic pregnancy is having suffered a previous ectopic pregnancy. Although the statistics are not conclusive, this risk would be around 10% as per the most recent study.
However, the key is to know what risk factors exist for a first ectopic pregnancy. Therefore, we can classify the risk factors into maternal, anatomical and embryonic.
Maternal risk factors
It seems that being a smoker, having a history of infertility, being of advanced age or taking a certain type of antidepressant (benzodiazepines) prior to pregnancy increases the risk of such a condition.
Anatomical risk factors
On the other hand, having had an infection in the tubes, called pelvic inflammatory disease, endometriosis, having used an intrauterine device (coil) as contraception or having had tubal ligation are considered as factors that increase the risk of ectopic pregnancy.
Nevertheless, in assisted reproduction treatments the synchronization of the endometrium with the development of the transferred embryo is taken into account. Avoiding the discrepancies between these two parameters, considered as one of the factors contributing to the appearance of an abnormal implantation, helps to achieve a physiological pregnancy. That is why a good endometrial preparation, with an adequate endometrial thickness, could avoid such condition. In this sense, embryo freezing is considered a strategy to follow.
Embryonic risk factors
More controversial is the classification of embryonic factors. However, a relationship has been observed between poor embryonic quality, low ovarian reserve and even, although still inconclusive, embryonic aneuploidies.
Diagnosis of ectopic pregnancy
Early detection of an ectopic pregnancy is essential to reduce morbidity and eventual mortality. It is based on a combination of:
- Measurements of human chorionic gonadotropin (B hCG) levels and
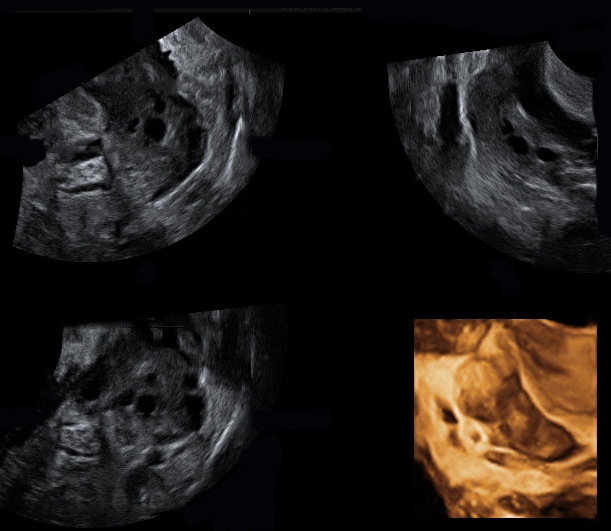
- Transvaginal ultrasound examinations
Under normal circumstances, with hCG levels of more than 1000-1500, an intrauterine gestational sac should be visualized. In addition, these hCG levels should double every 48 hours. Although this statement is true, an ectopic pregnancy should not be diagnosed without at least 3 hCG measurements and an inconclusive ultrasound. This is where the concept of pregnancy of unknown location (PUL) comes in. PUL is defined as a pregnancy confirmed by the presence of hCG in the blood without locating the gestational sac on ultrasound. Therefore, any PUL is an indication of possible ectopic pregnancy and is the first thing to be ruled out. Although the greatest fear of a PUL is the diagnosis of this event, it has been established at a frequency of 20% of all PULs.
There are three possible scenarios in the diagnosis of Ectopic Pregnancy
Pregnancy of unknown location or PUL
This situation requires a follow-up of hCG levels every 48 hours. An ectopic pregnancy may be suspected when these levels do not double as they should, but still, continue to rise. Ectopic nesting may also be suspected if in the ultrasound the endometrium is thin or if there is free liquid around one of the adnexa. Nevertheless, the definitive diagnosis is made after having done both three hCG measurements and the ultrasound examination. Sometimes it is necessary to perform a magnetic resonance imaging (MRI) to rule out less frequent intraperitoneal locations. This scenario is the most frequently found after an assisted reproduction treatment, since hCG levels are measured from a very early stages of implantation.
Ectopic pregnancy visible in the ultrasound
Although the levels of hCG need not be very high, a simple fact of visualizing an adnexal mass compatible with ectopic pregnancy is considered a feasible diagnostic. Sometimes it is even possible to see an embryo with a heartbeat in the fallopian tube or in other locations such as the cervical canal or isthmus. This situation occurs more frequently when the pregnancy has been conceived spontaneously.
Ectopic pregnancy rupture
This situation is considered as an emergency and should be attended immediately. It occurs with acute abdominal pain and blood in the peritoneal cavity visible by ultrasound. Therefore, this state is one that we wish to avoid by all means with early diagnosis and treatment.
Although attempts have been made to use other hormones such as progesterone for even earlier detection, the reality is that it has not proved useful for this purpose.
Ectopic pregnancy treatment
The management of ectopic pregnancy will depend on both the location of the pregnancy and its development. Therefore, basically and especially in tubal pregnancies, one of the three strategies will be chosen:
Expectant management
With a very early diagnosis and being the patient asymptomatic, it is possible to opt for an expectant management, since some pregnancies of this type simply perform an intraperitoneal or tubal miscarriage and with hardly any symptoms. This avoids any other type of treatment, although it is necessary to be very cautious and explain the risks to the patient. Likewise, a very strict control of the patient’s symptomatology, ultrasound and hCG levels are necessary.
Medical treatment with Methotrexate
This treatment is a chemotherapy that selectively eliminates the cells of the embryo. Although it is a widely used treatment for this purpose, it is not without flaws. Therefore, patients who can be offered it should be asymptomatic, no gestational sac with a heartbeat should be seen and, ideally, hCG levels should be below 1500 (although successful treatment has been reported up to 5000 level). It is also considered the ideal treatment for ectopic pregnancies of extratubaric location, especially those that affect the uterus, such as cornual, cervical or intramural ectopic pregnancies. It is important to note that after this treatment it is not possible to conceive until at least 3 months later.
Surgical treatment
Laparoscopy with the removal of the tube is the indication for tubal ectopic pregnancies when medical treatment is not possible or not indicated. Even more so when a rupture of the tube has occured. It is also necessary when it affects other extra-uterine locations where medical treatment is less effective, such as abdominal ectopic pregnancies
Other alternatives to consider may be embolization of the arteries that irrigate the uterus in those pregnancies that affect the uterus and where total removal of the organ is not desired.
Fertility after an ectopic pregnancy
Although it seems logical to think that fertility can be impaired by the appearance of this complication, it is a controversial issue, and not only dependent on its mere appearance but also on the age of the woman and whether there is a concomitant pathology such as endometriosis.
However, future fertility does not seem to depend on the treatment chosen in its management. Although it should be noted that patients over 35 years old or with a fertility history that has not been subjected to the removal of the tube will be more likely to have a second ectopic pregnancy. On the other hand, it must be taken into account that the implantation of an embryo in the tube can produce an obstruction of that tube and reduce the chances of gestation.
A recent study has shown that patients, who have suffered this condition, even if they have an intrauterine pregnancy, have a higher risk of suffering from certain obstetric pathologies such as premature birth, placenta praevia or placental abruption.
In vitro fertilization and ectopic pregnancy
In vitro fertilization (IVF) has always been considered a risk factor for ectopic pregnancy.
It is well known that patients who are undergoing in vitro fertilization have the most important risk factors for the appearance of ectopic pregnancy such as endometriosis, previous pelvic inflammatory disease, endometrial pathology that prevents normal intrauterine implantation as intrauterine adhesions or adenomyosis.
Therefore, in order to avoid such circumstances, it has already been observed that reducing the culture medium with which the embryo transfer is made, performing it at a prudent distance from the uterine fundus and the cervical canal and focusing on good endometrial preparation is effective. Moreover, embryo freezing has been considered a strategy for patients at high risk of ectopic pregnancy.
Dr Belén Moliner, gynaecologist at Instituto Bernabeu
IT MAY ALSO BE OF INTEREST TO YOU:
- Implantation failure and recurrent miscarriage Unit in Instituto Bernabeu
- What is a Chemical Pregnancy?
- Molar pregnancy or hydatidiform mole
- Anembryonic gestation
- Pregnancy check-ups and labour
