Infections in testicles or reproductive tract that can cause male infertility: epididymitis, orchitis and STIs.
Infection of the male urogenital tract is a potentially curable cause of male infertility. WHO considers urethritis, prostatitis, orchitis and epididymitis to be infections of the male accessory glands.
Índice
- 1 How can I tell if I have a testicular or reproductive tract infection?
- 2 What types of infection can we find in the testicle?
- 3 How can this testicular infection be detected?
- 4 How can this kind of testicle infections affect fertility?
- 5 Which would be the treatment for these male reproductive tract infections?
How can I tell if I have a testicular or reproductive tract infection?
To know if I have a testicular or reproductive tract infection, we can check the presence of:
- Testicular pain
- Constant or intermittent discomfort
- Feeling of heaviness
- Urethral pain or burning
- Perineal pain
- Occasional fever and/or very characteristic scrotal swelling
What types of infection can we find in the testicle?
In most cases the infection will come from the bladder or prostate with a previous infection spread through the seminal tract to reach the testicle. Thus urethritis, urinary tract infections and prostatitis are in many cases the origin of bacterial orchitis. Viral orchitis has other mechanisms, such as the mumps virus, which causes infertility.
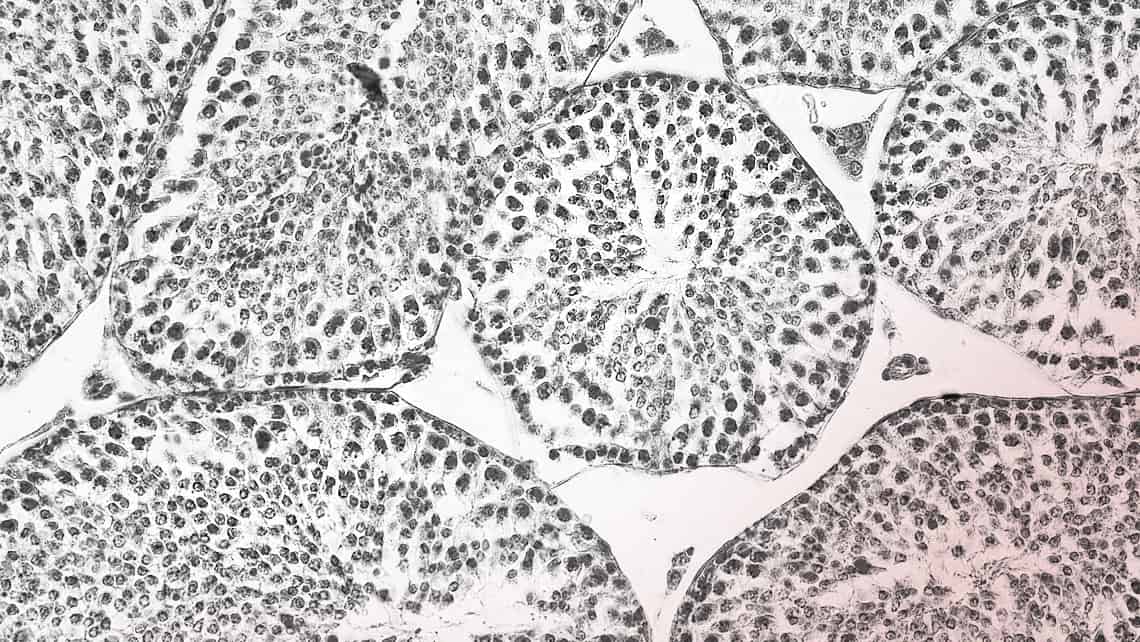
How can this testicular infection be detected?
These infections can be detected by means of a physical examination, showing an increase in the size of the testicle and its appendages. The study will be completed with:
- Urine analysis
- Semen culture
- Ultrasound scan of the testicle and the rest of the urinary tract, including bladder and prostate, to determine the extent of the infection or its evolution.
- The study of the seminogram and seminal fluid also helps in the diagnosis.
The European Association of Urological Clinical Practice Guidelines 2022 (EAU2022 Guidelines) describes advances in the relationship between genitourinary tract infections and infertility which are detailed below:
- Once the urinary tract infection UTI (including urethritis) is excluded, the presence of elevated white blood cells in the ejaculate indicates an inflammatory process. In these cases it is useful to perform a sperm culture or PCR analysis to identify and classify the germs affecting the urinary or sperm tract.
- A high concentration of >103 CFU/Ml urinary tract pathogens in the ejaculate is indicative of significant bacteriospermia or infection, and this is the most accurate method. The sample should be shipped the same day to the laboratory as a delay in the delivery will influence the rate of positive microorganisms in the semen and the frequency of isolation of different strains.
How can this kind of testicle infections affect fertility?
Recently, it has been discovered that the uretral or prostatics infections caused by Ureaplasma Urealyticum and Mycoplasma hominis are related to infertility, but the Ureaplasma parvum and Mycoplasma genitalium bacteria were not related to male infertility.
Frequency of human papillomavirus (HPV) in sperm ranges from 2 and 31% in the general population and is highest in men with unexplained infertility (10-35.7%). Recent reviews have reported an association between male infertility and the presence of this virus, as well as poorer pregnancy outcomes and HPV positivity in semen. However, data still need to be validated to clearly define the clinical impact of HPV infection in sperm.
Moreover, the seminal presence of Herpes Simplex virus (HSV)-2 in infertile men may be associated with lower sperm quality compared to that of HSV-negative infertile men, and it is unclear whether antiviral therapy improves fertility rates in these men.
Which would be the treatment for these male reproductive tract infections?
Treatment of male accessory gland infections may improve clinical symptoms, including sperm quality, but doesn’t necessarily improve the likelihood of increased conception, and this is a fact.
It is appropriate to refer sexual partners of patients with known or suspected sexually transmitted infections of the accessory sex glands if it is known or suspected to be caused by N. gonorrhoeae or C. trachomatis for evaluation and treatment.
Treatment of epididymitis results in microbiological cure of the infection, improvement of clinical signs and symptoms, prevention of possible testicular damage, prevention of transmission and reduction of possible complications such as infertility or chronic pelvic pain.
Dr Luís Prieto, director of urology at the Instituto Bernabeu
