Septate Uterus: what it is, how it is diagnosed, and its treatment
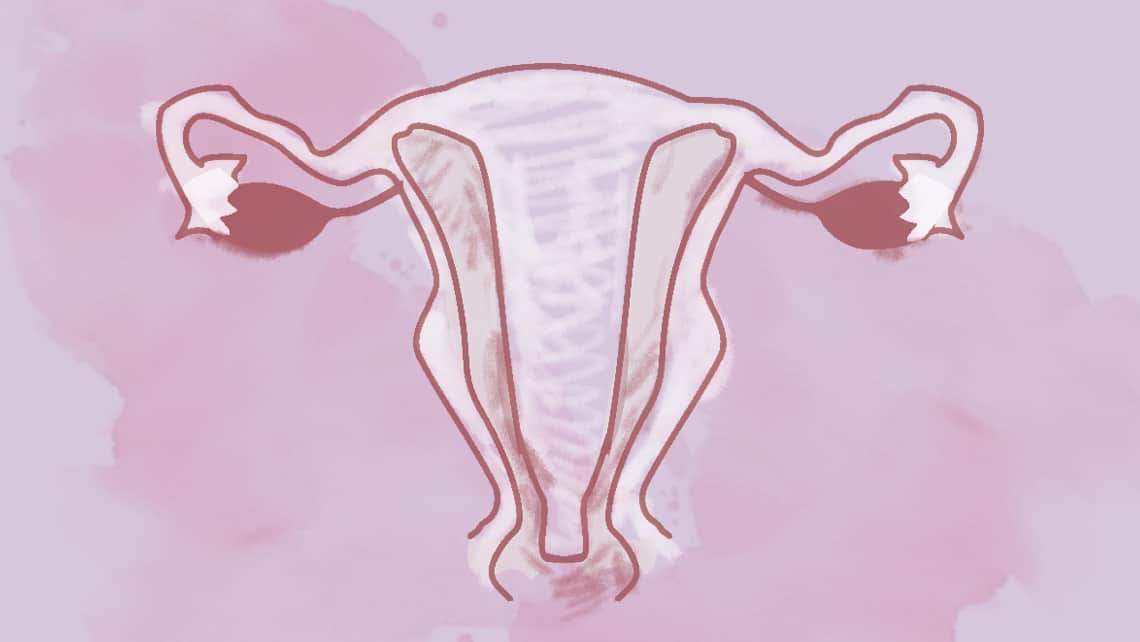
The uterus, fallopian tubes and vagina (or at least part of it) come from embryonic structures called Müllerian ducts. These are two tubular formations which appear on each side of the body, which join at the centre at around the 10th week.
At around 20 weeks, the septum separating both ducts must be reabsorbed, and it is in this process when septate uteri form as a result of failure of reabsorption which may lead to different types of septa or partitions:
- Partial septum: The septum does not cover the entire uterine cavity; we therefore find connection between both halves.
- Complete septum: The septum reaches the internal cervical os, completely dividing the uterine cavity in two.
Septa are not only found in the uterus; this failure in reabsorption may continue and be seen in the cervical canal and even in the vagina.
As these ducts also participate in the formation of other organs, whenever we find a Müllerian malformation, vaginal and kidney malformations must be ruled out.
It is the most common Müllerian anomaly with an incidence which may reach 2-3% in women, the rate being higher if we focus on women with fertility problems.
Índice
How are septate uteri diagnosed?
The two techniques which best help us diagnose whether there is a uterine septum are 3D ultrasound and magnetic resonance. With these we can see not only whether or not there is a septum, but also whether it is complete or partial, and its thickness, with a view to potential surgery. It also helps us to distinguish septa of didelphic uteri and to see whether the renal system has any associated malformation.
Another option would be undertaking a diagnostic hysteroscopy which allows us to assess the cavity and potential subsequent surgery, but this has the disadvantage of not allowing us to see the uterine contour, and we could therefore confuse a septate uterus with a bicornuate uterus or didelphic uterus.
What symptoms can the septate uterus cause?
In daily life, patients with septa do not usually have symptoms, such as pain during menstruation, hypermenorrhoea or heavy bleeding. They have been related with an increase in obstetric and reproductive complications, above all with complete septa, for example:
- Increased rate of miscarriage in both the first and second trimester.
- Abnormal foetal position.
- Increased rate of caesarean due to these abnormal positions.
- Greater risk of preterm birth.
- Alterations of placentation which may lead to the appearance of intrauterine growth retardation (IUGR) and placental abruption.
In the case of the partial septate uterus, although these complications may appear, their relationship is not always as significant. The subseptate or arcuate uterus must also be mentioned, in which these associations do not appear; today, the latest classifications of Müllerian malformations consider them a variation of normality, although there are different criteria for definition.
Why do these complications occur when the septate uterus is diagnosed?
It is believed that there are multiple causes:
- Alteration in the vascularisation of the endometrium
- Distortion of the uterine cavity and reduction of its volume
- Alterations of contractility and distensibility
It must be indicated that a woman with a septum may become pregnant and give birth without experiencing these effects; there is therefore still debate over whether or not ALL septa should be operated on. As always, it is important to PERSONALISE each case, as there is not a single solution for everyone.
What is the treatment for the septate uterus?
The only corrective treatment is septoplasty; that is, removing the septum with a procedure called hysteroscopy. It has been observed that the removal of the septum may reduce the risk of miscarriage and abnormal foetal position; therefore it would be suitable for patients with a history of recurrent pregnancy loss or a previous history of obstetric complications due to foetal position. It has not been shown to improve implantation rates, therefore, as we have mentioned, each case must be personalised, because all interventions have potential complications.
Dr María Martínez gynaecologist at Instituto Bernabeu
