What are the main causes of embryo implantation failure?
The reproductive process comprises a series of events among which implantation is one of the most critical. For implantation to take place correctly, the following are necessary: a competent blastocyst, a receptive endometrium and correct communication between them.
When implantation repeatedly fails to occur, this is known as recurrent implantation failure (RIF) and is a tremendously frustrating situation for both patients and physicians. Its treatment is one of the greatest challenges in the field of assisted reproduction.
Índice
What is embryo implantation?
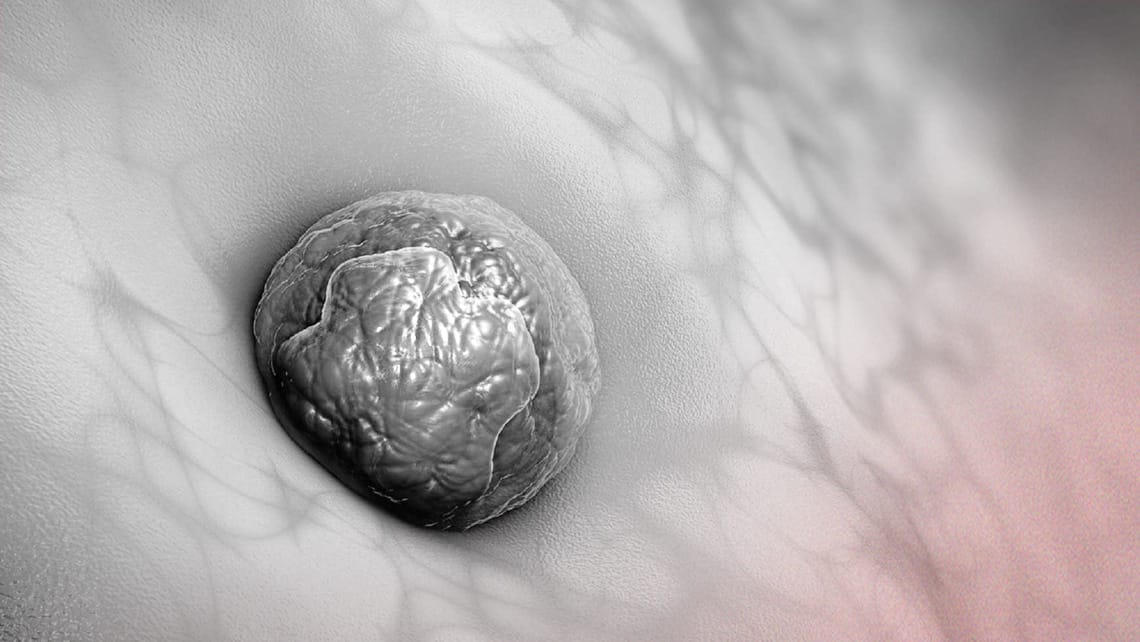
Implantation is the process by which the blastocyst stage embryo attaches to the maternal endometrium, initiating gestation. It consists of 3 phases: apposition, adhesion and invasion. During apposition, the embryonic cells come into contact with the endometrial epithelium. Later, during adhesion, the blastocyst anchors itself to the outermost layers of the endometrium and then completely invades the endometrial tissue.
After assisted reproductive techniques, implantation is usually confirmed by ultrasound with visualisation of the gestational sac.
When can we diagnose embryo implantation failure?
There is currently no agreed definition for recurrent implantation failure (RIF). It is a condition arising from the failure of a successive number of in vitro fertilisation (IVF) cycles in which pregnancy should theoretically already have been achieved. Due to the enormous variability between different assisted reproduction centres, a consensus definition for this event has not been achieved.
However, today the most accurate definition of RIF could be considered as the failure to achieve a positive result after transfer of at least 3 good quality blastocysts in women up to 37 years of age or 3 euploid blastocysts in women older than 37 years of age.
What are the causes for embryo implantation failure?
Generally speaking, the causes of implantation failure can be categorised as embryonic, uterine and systemic.
- Embryonic:
We know that the embryo chromosomal status influences its ability to implant correctly. Chromosomally normal (euploid) embryos, regardless of maternal age, have a lower rate of implantation failure.
In addition to embryonic euploidy, other genetic alterations such as mutations or alterations in methylation may have an impact, as yet uncertain, on implantation failure.
In addition to genetics, embryo quality also plays an important role in implantation from a morphological point of view. Regardless of other factors, an embryo categorised as good quality has a higher implantation potential than an embryo of lower morphological quality.
- Uterine:
In addition to the embryo potential, an adequate and receptive uterus is of utmost importance for implantation to occur properly. Some of the uterine anomalies that can negatively affect implantation are:
- Mullerian malformations such as septate or T-shaped uterus.
- Anatomical pathologies such as synechiae, endometrial polyps or myomas.
- Presence of thin endometrium
- Adenomyosis
- Chronic endometritis and alteration of the endometrial microbiome.
- Presence of increased uterine peristalsis.
- Systemic:
After the experience acquired and after the large number of studies carried out on the subject, it has been concluded that implantation is a highly complex process in which there are two clear protagonists (embryo and uterus) but which involves a series of factors at the systemic level that could be determinant.
Among the most studied systemic alterations for their possible implication in implantation failure are thrombophilias, immunological alterations and those related to lifestyle.
What are the possible solutions to implantation failure?
As previously described, the possible causes of recurrent implantation failure are numerous and some have yet to be determined, so finding a generalised solution to this condition is particularly complex.
Following the many studies published on the subject and following the recommendations proposed by the SEF (Spanish Fertility Society) working group on reproductive failure, the following should be evaluated:
- Pre-implantation genetic screening (PGT-A): transfer of chromosomally normal embryos and less time to achieve gestation.
- Blastocyst stage transfer: provides better embryo selection and generates more information on the quality of the embryo to be transferred.
- Assisted hatching: there are publications that indicate that assisted hatching could favour embryo implantation in cases of RIF. When performed before the embryo biopsy, it would be included in the PGT-A.
- Study of thrombophilias: the study of antiphospholipid antibodies in patients with RIF should be individualised (taking into account possible personal or family history of autoimmune diseases).
- Study of immunological causes: there are no defined immunological markers related to RIF and there are no immunological treatments that improve prognosis.
- Ovarian stimulation: in cases of hyper-responsiveness to ovarian stimulation it is recommended to avoid fresh transfer, freezing the embryos for a deferred cycle.
- Promoting a healthy lifestyle may improve the prognosis in the patient undergoing assisted reproduction techniques.
- Hysteroscopy should be performed when there is suspicion of pathologies that can be corrected by this technique, such as septate uterus, subseptate uterus and T-shaped uterus. Correction is also recommended in the case of endometrial synechiae or polyps (especially if they are larger than 10 mm) as well as submucous myomas or intramural myomas that deform the uterine cavity.
- Endometrial receptivity test. It is based on a possible desynchronisation between the endometrium and the embryo as a consequence of the displacement of the window of implantation. However, there is no evidence for its systematic recommendation at present.
- In cases of absence of euploid embryos or embryo blockage, egg donation is proposed as a solution to the embryonic cause of RIF.
Laura Cascales, biologist at Instituto Bernabeu
