Implantation failure and repeated miscarriage unit
Implantation failure requires a specialized treatment that is provided at Instituto Bernabeu by a specific multidisciplinary unit.
What is implantation failure?
It is defined as a failed attempt to achieve a viable pregnancy by means of IVF.
That is, it encompasses both those patients who fail to become pregnant and those patients who become pregnant but have an early miscarriage.
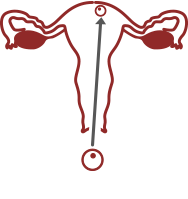
NORMAL IMPLANTATION
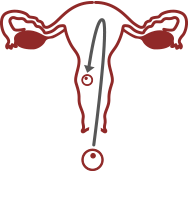
IMPLANTATION FAILURE
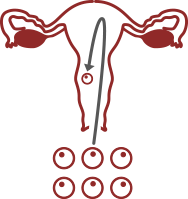
REPEATED MISCARRIAGE
Why does embryo implantation failure happen?
It is a challenge to answer this question because we are unaware of many processes that result in a successful embryo implantation.
To begin with, it must be kept in mind that the cause cannot be attributed to a single patient (the mother) but to THREE: the mother, the father and the embryo.
We do know that some causes are related to the mother, but most of them have to do with the embryo, and not always can it be diagnosed or treated successfully. Hence the patient’s high degree of uncertainty and anxiety when doctors are not able to find the failure causes.
Nevertheless, great progress has been made in this field over the last years.
An accurate study of implantation failure requires a multidisciplinary assessment. For this reason, a working group that specializes in these disorders was created at INSTITUTO BERNABEU. This group includes gynecologists, endocrinologists, molecular biologists, geneticians and embryologists.
An analysis for diagnosing embryo implantation failure and recurrent pregnancy loss
 Female factor
Female factor
Whilst we still have a long way to go before we fully understand the female factors that explain implantation failure and recurrent pregnancy loss, there have been some new findings on the subject.
Three-dimensional ultrasound scans performed by expert sonographers plus sophisticated equipment mean that it is possible to rule out adenomyosis, a well-known cause of endometrial receptivity loss and anatomical abnormalities in the uterus.
However, immunology analyses rarely help and any treatment derived from these analyses often fails to have a positive impact of any kind. That said, and taking into account the fact that this field is in continuous development, we have a Reproductive Immunology Department at IB that assesses this factor and carefully monitors any progress that is made.
We also carry out studies on uterine contractions when embryo transfer takes place. We must not forget that the uterus is a muscle and, therefore, any inappropriate stimulation of the uterus increases contractions that could lead to expulsion of the embryo. The detailed progress of our uterine contractility study has been published in the prestigious journal Fertility & Sterility.
An ultrasound video studying contractions and measuring progesterone levels is incredibly useful in ruling out and treating this cause.
Last of all, at Instituto Bernabeu we are undergoing studies on the efficiency of placing substances that stimulate the endometrium inside the uterine cavity days before transfer in order to increase biological competence
Intrauterine HCG: the instillation of HCG into the uterine cavity prior to embryo transfer with the purpose of increasing endometrial receptivity.
Intralipids: The administration of intralipids around the time of transfer and after the achievement of pregnancy can help to increase the percentage of implantation and, on the other hand, decrease the miscarriage probability. (Learn more)
It is clear to see that analysing the maternal factor calls for a multiple assessment approach.
We also perform a study called IBgen RIF that includes a genetic, immunological and haematological factor panel meaning that a single test can provide us with information about different causes. After the study of the specific case, it may also be recommended to perform massive sequencing panels (NGS). More information
Our most recent research work has demonstrated the impact of the microbiome (the microorganisms that live around the genitalia) on fertility. This prompted us to begin analysing it so that measures can be taken if abnormal results are obtained. (Learn more).
At the same time, another technique that has shown its benefits in carefully selected cases is the intrauterine application of platelet-rich plasma (PRP). Recent studies have shown good results on the role of platelets in the repair and regeneration of different tissues in patients with recurrent embryo implantation failure and in women with refractory endometrium. The use of platelet-rich plasma from the patient herself could improve endometrial receptivity and, consequently, implantation. (Learn more)
 Male factor
Male factor
The MALE FACTOR is studied through the karyotype, DNA fragmentation, an andrology-based exploration and chromosome assessment.
A karyotype (study of the chromosomes number and arrangement) performed on blood cells can return an entirely normal result. However, this may not be the case for the spermatozoa chromosomes. This is why we include a test called FISH in the analyses. This test assesses an elevated number of spermatozoa, usually more than 1000, to find out what chromosomal endowment it carries.
Your gynaecologist may recommend a testicular meiosis study if your sperm parameters are abnormal, which may be the potential cause of previous unsuccessful attempts at in vitro fertilisation techniques, implantation failure or spontaneous pregnancy loss.
In meiosis, spermatozoa precursor stem cells split their genetic load in half and change from having 46 chromosomes to 23. If there are abnormalities during this phase, they can affect the gamete’s chromosomal make-up and, consequently, cause fertilisation failure, abnormal embryo development, implantation failure and premature pregnancy loss.
The procedure generally entails taking a small testicular biopsy although analyses can sometimes be performed on ejaculate. The result helps to ensure that the most suitable decision regarding reproduction can be taken.
 Embryo factor
Embryo factor
However, the EMBRYO FACTOR is undoubtedly the area in which most progress has been made.
It is clearly responsible for most cases of implantation failure and recurrent pregnancy loss.
We should not forget that the embryo stems from the combination of two reproductive cells: the spermatozoon and the oocyte. Therefore, exquisite care when it i being processed, strict development tracking, culture conditions in the laboratory, and the delicate transfer to the mother’s uterus must be taken into account when explaining previous failures.
Nowadays, molecular and biology genetic techniques make it possible to analyse all of the embryo’s chromosomes, as the most common cause for implantation failure and early miscarriage is an abnormal number and constitution of the embryo’s chromosomes.
The transfer of chromosomally normal embryos makes pregnancy rates remain the same regardless of the mother’s age. At the same time, miscarriage risks decrease dramatically. In other words, whenever embryos that are free from chromosomal abnormalities are transferred, patients will always have the same expectancy for success regardless of their age.
This technique, known as Pre-implantation genetic diagnosis or testing (PGD/PGT), is used around the fifth day of the embryo’s development and is proving to be greatly effective to answer the most relevant questions for patients and for the doctors that take care of them. Why do embryos fail to implant? Why do they miscarry? Is the treatment worth repeating? Is it time to leave it or change it?
Comprehensive Analysis 1 day. 100%
 Female partner
Female partner
- Personalised analysis of your medical history
- Hysteroscopy and endometrial biopsy. Functional study of the endometrium and CD138 antibody marker for a specific analysis of chronic endometritis
- Implantation failure genetic risk profile
- Tests for thrombophilia
- Immunological tests
- Thyroid function tests: TSH and anti-TPO
- Karyotype
- Vitamin D
- Genital microbiome analysis
- Evaluation of the uterus using high-resolution ultrasound imaging
- Study, if appropriate, of uterine contractility and progesterone levels on the day of embryo transfer
 Male partner
Male partner
- Karyotype
- DNA fragmentation study (TUNEL)
- Sperm FISH
 Embryo profiling
Embryo profiling
- PGS/PGT-A/CCS
- Personalized analysis of your medical history