Infertility and male sterility
30% of problems in achieving pregnancy originate in the male partner. Numerous solutions are currently available, and in most cases the use of donor semen from the sperm bank is not necessary.
When couples are infertile, it means that both partners need to undergo a study. The male partner is directly involved in almost half of all cases of sterility – the inability to conceive. Infertility is the name given to cases of men who are unable to have children. In many cases, this is due to a reduced number of spermatozoa.
There are two types of male infertility: complete infertility, meaning that a man cannot have children, which affects one in every 500 men; and relative or subfertility which means that a man needs more time than is considered normal in order to achieve a pregnancy.
What can cause male sterility?
The cause may be congenital (the man is born with it), as is the case of anatomical or hormonal disorders and malformations of the sexual organs. Or there may be external causes: toxic habits such as the consumption of and exposure to drugs, genital infections, pharmaceutical drugs, radiation or environmental contaminants.
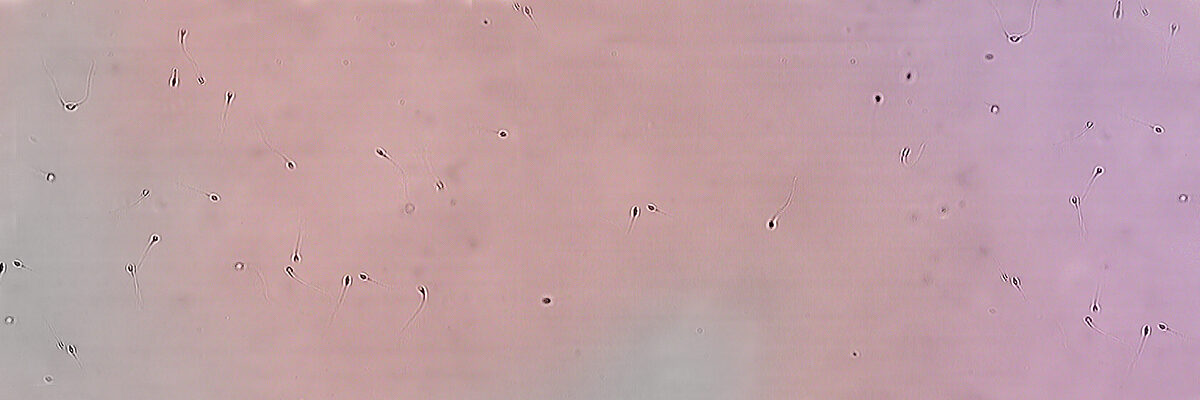
The main issues are abnormalities in semen parameters with no apparent or identifiable reason. That is, having a low number of spermatozoa (oligozoospermia), sperm with poor mobility or reduced motility (asthenozoospermia)or abnormal morphology (teratozoospermia), amongst others.
There may also be more specific and more identifiable semen abnormalities such as obstruction issues in the seminal tracts, infections, genetic reasons which interfere with egg fertilisation or embryo quality, as well as specific illnesses which have an impact on the ability to reproduce.
It is not uncommon for a man to want to have a child after having had a vasectomy. In the majority of cases, assisted reproduction will be necessary in order to retrieve spermatozoa. Nowadays, such procedures are not in any way complicated.
When should you turn to your specialised doctor for advice?
When a pregnancy is not achieved following a period of sexual intercourse without the use of contraceptives: around one year if the female partner is under 35 years of age; around 6 months if she is aged between 35 and 40; and very soon after beginning to try for a child if she is aged over 40. Of course, no time at all should be lost in those cases in which the male partner’s medical history is an indicator. For example, cases of men who were operated on as a child in order to correct genital malformations – hypospadias (affects the penis), cryptorchidism (incomplete or failure of the testes to descend in the scrotum) – or if there are issues during sexual intercourse.
Up until a few decades ago, the options for treatment were few and far between and making use of a semen bank was the only option. Nowadays, thanks to IVF (in vitro fertilisation) and ICSI (intracytoplasmic sperm injection) and related techniques for obtaining spermatozoa through the testes, spermatozoa can be obtained using techniques that are increasingly more sophisticated. For example, FNA (Fine Needle Aspiration) and testicular biopsies, thus limiting the use of donor semen to just a few cases.
Tests for studying and evaluating male sterility
A consultation with a specialist is an essential part of the study process since, based on this, we are able to select the specific tests which will provide us with useful information. During this exchange with the doctor, anything which may be affecting semen quality must be researched. For example, cases of sterility in the family, exposure to toxins, lifestyle, etc.
A seminogram is an essential test. It is easy to carry out and provides us with a lot of information for deciding on the course of treatment and requesting other complementary tests.
An urological examination is also important in males with semen abnormalities or functional impediments. An andrologist will recommend the best technique in order to optimise results during assisted reproduction treatment or even without having to turn to treatment of this kind.
Chromosome and genetic studies in blood and in sperm samples (TUNEL, FISH, sperm meiosis…) would complete the usual tests carried out on men, should they be necessary.
In addition, at Instituto Bernabeu we have a new diagnostic test –IBgen SPERM– to analyse the full complexity of the sperm formation process (spermatogenesis) and to find out the origin of genetic infertility.
Treatment for sterility should never begin based solely on a seminogram and no thorough analysis of the male partner. Many courses of unnecessary insemination or in vitro fertilisation treatment have been carried out in this way!
COMPLEX MALE FACTOR STUDY
We investigate the origin to find the solution
We have developed a complete study for patients with Severe Male Factor. It includes the main tests which will reveal the origin of the male infertility. It is notable for our exclusive genetic study based on the massive sequencing of 426 genes involved in the synthesis and maturation of spermatozoa to ascertain whether there are alterations. This is valuable information to allow assessment of the prognosis and even adoption of measures for preservation of fertility.

The NEW TEST consists of a set of analyses which fully and thoroughly study the male factor
The tests included are:
- Karyotype
- Y chromosome microdeletion
- FISH in spermatozoa
- TUNEL
- Male factor NGS panel
- Urologist consultation
- Genetic test
The study is recommended for patients who do not produce spermatozoa in ejaculate (azoospermia), or who have an abnormally low number, one million per millilitre and more serious cases of under 100,000 per millilitre (cryptozoospermia).