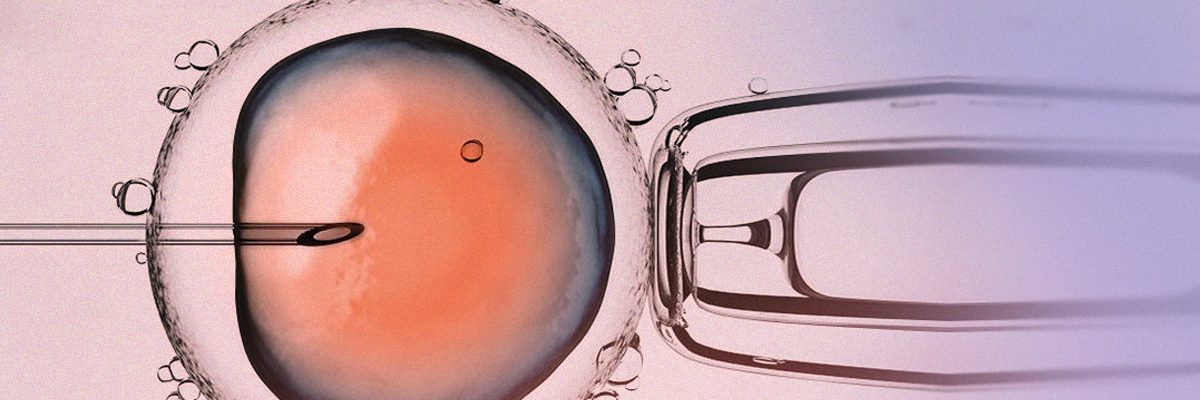
ICSI: Intracytoplasmic Sperm Injection
Injecting a single sperm into a mature oocyte facilitates fertilization
What is ICSI?
Intracytoplasmic Sperm Injection (ICSI) is performed by injecting a single sperm into a mature oocyte to achieve fertilization. This is no doubt the most commonly used assisted reproduction technique (ART). It proved a real revolution at the beginning of the 90s, since it successfully solved most masculine infertility problems.
Because of its high and constant success rates to achieve fertilization (70-80%), the ICSI technique has not significantly changed since it began to be used. The necessary equipment features an inverted microscope, with specific optics and a heating stage to maintain the temperature at 37ºC/98ºF. A number of 3D micromanipulators are attached to the microscope to move the micropipettes holding the oocyte and containing the sperm. Sperm motility and the experience of the embryologist applying the technique are two of the most important parameters to guarantee its effectiveness.
When is ICSI advised?
Advising ICSI should follow from a comprehensive fertility assessment of both partners. For instance:
1. Masculine sterility:
- Oligozoospermia or cryptozoospermia: A severely low sperm count.
- Astenozoospermia: A severely low sperm motility, including samples with a total lack of motility.
- Teratozoospermia: A high number of abnormal sperm.
- Obstructive azoospermia: A total absence of sperm in the ejaculate due to an obstruction. The most common causes are genetic disorders, inflammation and failed vasovasostomy.
- Testicular azoospermia: A total absence of sperm in the ejaculate due to a disorder of sperm production in the testicles.
- Anejaculation: Ejaculatory dysfunction caused by retrograde ejaculation or paraplegia.
In cases of azoospermia and anejaculation, the sperm needed for ICSI can be retrieved directly from the testicles (by testicular puncture or biopsy).
- Immune cause: presence of high levels of antisperm antibodies.
- Valuable sperm samples: patients who freeze their sperm sample before undergoing chemo- or radiotherapy, patients who require sperm washing because they have an infectious disease (HIV, hepatitis) or use donor semen.
2.Female sterility:
- A low oocyte count is retrieved after the follicles are punctured. In cases like this, standard IVF can be performed.
- The quality of oocytes is low in general, including the swollen oocyte coat (zona pellucida).
3. Other causes:
- Long term infertility (more than 2 years trying to conceive).
- Several unsuccessful cycles of timed intercourse or artificial insemination.
- Not performing standard IVF in a previous cycle.
- Rescue microinjection: oocytemicroinjection for having failed to fertilize after standard IVF.
- In Vitro Oocyte Maturation.
- Failing to achieve pregnancy after several standard IVF cycles.
- Performing PGS/PGT-A/CCS or DGP.
- Vitrified oocyte microinjection.