Poor Ovarian Responders Treatment Unit
With age, there is a lower oocyte quantity and quality resulting in more difficulties when trying to conceive naturally, in addition to failure when using traditional assisted reproduction techniques.
What is the ovarian response?
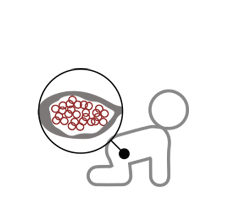
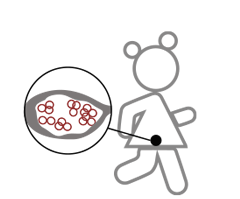
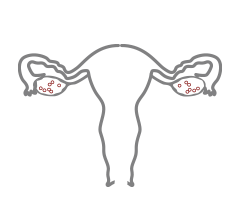
One of the most important phases during any IVF treatment is ovarian stimulation. In this phase, patients are required to take medication for a period of between 7 and 12 days in order to obtain several oocytes for fertilisation. Therefore, ovarian response is defined as the quantity of oocytes obtained following the above stimulation. This is carried out in order to obtain an adequate amount of oocytes to guarantee favourable embryo prospects. In general terms, an amount of 5 oocytes is considered adequate.
However, we can obtain very different responses from patients who are subject to identical medication doses. In some cases, the total quantity of oocytes is so low that any chances of success are considerably reduced. These cases are referred to as poor ovarian response.
What is the ovarian reserve?
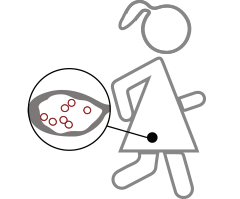
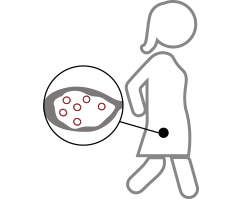
Women are born with the entire amount of oocytes that they will have during their whole life. As time passes by, these oocytes will be lost until they completely run out with the onset of menopause.
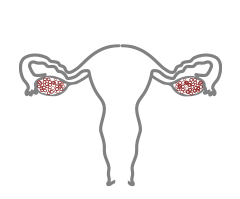
Therefore, ovarian reserve is defined as the total quantity of suitable oocytes available in a woman’s ovaries at any given time, which shall determine the amount of oocytes that can be obtained during IVF treatment. When it comes to measuring a woman’s ovarian reserve, the antral follicle count by ultrasound and the anti-Mullerian hormone (AMH) level tests are the most reliable indicators.
Although a low ovarian reserve is the main cause of poor ovarian response, this can also happen in women with otherwise normal ovarian reserves.

What are the causes for low ovarian reserve?
As previously indicated, ovarian reserves reduce progressively with age until they completely run out. For that reason, age is one of the main risk factors when it comes to low ovarian reserves. However, reserves can greatly vary even among women of the same age, with some women showing a low reserve earlier than others. Likewise, it is not uncommon for some over 40’s to have a normal reserve and high ovarian stimulation response, therefore resulting in a high amount of oocytes available for IVF treatment. This is due mainly to genetic but also environmental factors.
In these regards, at Instituto Bernabeu’s Poor Responders Unit we are currently working on several research studies in order to develop genetic tests that can predict whether a specific woman is at risk of losing their ovarian reserve sooner,among other research areas.
Why is the problem of low ovarian reserve so important in the search for pregnancy today?
Social changes in the last few years have resulted in women being forced to delay motherhood. From the age of 35 years old onwards, these women are affected not only by a reduced ovarian response, but also by a considerable progressive decrease in the amount of oocytes. Due to the relationship between age and the ovarian reserve, we have an increasing amount of patients with poor ovarian response to stimulation, resulting in a negative prospect when it comes to IVF treatment. Often referred to as Poor Responders, these are patients are most crucially in need of a correct assessment in order to define the best strategies to follow in order to increase the chances for a successful pregnancy.
LOW RESERVE
LOW OVARIAN RESERVE
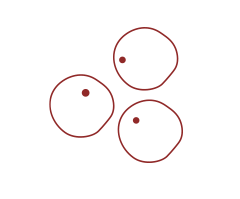
LOWER RESULT THAN STIMULATION

FERTILIZATION
EVOLUTION OF THE CROP
EMBRYONIC DEVELOPMENT DAY 5
NO TRANSFER
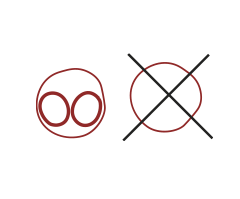
NORMAL RESERVE
NORMAL OVARIAN RESERVE
OPTIMAL RESULT TO STIMULATION
FERTILIZATION
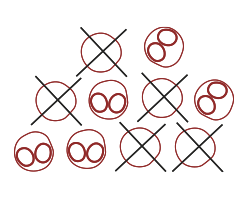
EVOLUTION OF THE CROP
EMBRYONIC DEVELOPMENT DAY 5
REMAINING TRANSFER AND FREEZING

Independent low ovarian reserve unit
Instituto Bernabeu’s Poor Responders Independent Unit
At Instituto Bernabeu we confronted this challenge within the reproductive medicine field in order to improve our patient’s chances to get pregnant with their own eggs by creating a pioneering Unit to treat poor responders. As the first unit of its kind in Spain, we have treated couples from several countries all over the world.
Our multidisciplinary unit comprises a team of practitioners specialising in reproductive medicine, molecular biology, genetics and reproductive biology with the purpose of assisting these couples while offering assistance and research in order to provide a customised treatment plan that is unique for each patient.
What does the Poor Ovarian Reserve multidisciplinary approach consist of?
All cases dealt with at this Unit are analysed and discussed by a team of specialised professionals. The fact that they have access to the IB’s low ovarian response unit from the very first appointment allows patients to benefit from the latest innovations in diagnosis and treatment: specific and cutting edge laboratory tests, 4D gynaecology ultrasound scans for ovarian and uterine research, genetic markers, prognosis and Array-CGH are some of the tests used to design a customised strategy aimed at improving every couple’s chances for success.
Advantages of Instituto Bernabeu’s Low Ovarian Reserve Unit
Access to top professionals and the most advanced diagnostic techniques makes it possible to individually define the most appropriate strategies for each case and improve the pregnancy success rate.
We apply pharmagenetics:
- Analysis of the genes associated with ovarian reserve allows us not only to diagnose, but also to define the most appropriate medication for each patient, optimising their ovarian response to stimulating hormones (IBgen low reserve).
- Fertigenetic study of massive sequencing to identify the mutations associated with ovarian failure to provide a correct diagnosis with which to individualise the most appropriate assisted reproduction treatment in the case of premature ovarian failure (early menopause): IBgenFOP.
On the other hand, our experience when dealing with complex cases has helped us to better understand the emotional baggage of our Poor Responder patients in situations where further sensitiveness is required, as well as emotional care.
Over the last few years, our Unit has developed and perfected the most innovative stimulation protocols. From adjuvant therapies to improve ovarian sensitivity to double stimulation in the luteal phase, as well as the accumulation of oocytes or vitrified embryos to the use of soft protocols, all the above techniques have been implemented in order to obtain promising results in patients who would otherwise be required to find an oocyte donor.
Ovarian rejuvenation
Platelet-rich plasma and growth factors
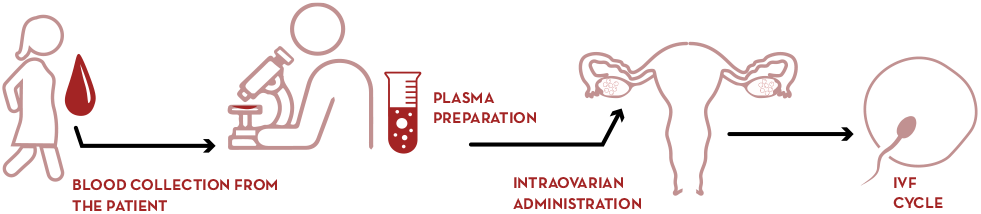
- Administration of the patient’s own platelet-rich plasma (PRP) to the ovary to promote the activation of “dormant follicles” and increase egg retrieval in patients with low ovarian reserve. Learn more
Administration of the patient’s own platelet-rich plasma (PRP)
Autotransplantation of the ovarian cortex
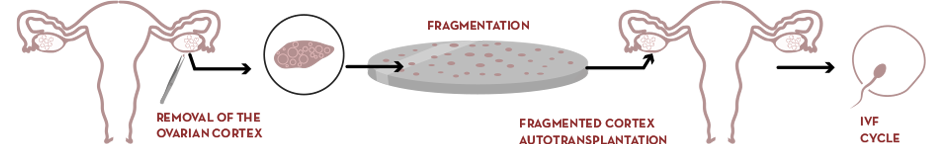
- Ovarian activation through ovarian cortex fragmentation and autotransplantation to achieve ovarian response in patients with ovarian failure or early menopause. Get more information
Ovarian cortex fragmentation and autotransplantation
Frequently Asked Questions about Ovarian Rejuvenation
- Our specialists answer the 12 most frequently asked questions about ovarian “rejuvenation.”
These procedures, still in the experimental phase, are aimed to “activate” the oocytes that remain “dormant” in the ovary and are resistant to the drugs used in ovarian stimulation.
They are aimed at obtaining eggs in patients with early menopause or increasing their number in patients with low ovarian response. The results obtained in the studies carried out so far are promising, opening up a line of hope in patients with a poor prognosis.
Ovarian reserve is determined from birth and decreases in number and quality until menopause. In fact, 5 to 10 years before the final menopause, most eggs are not capable of producing competent embryos.
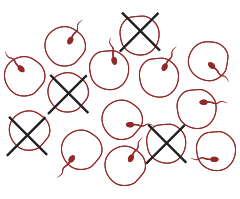
Therefore, the eggs quality in a treatment depends mainly on the age at the time of retrieval, although there are some pathologies that may influence.
Unfortunately, there is no treatment to improve the eggs’ quality, neither are the new ovarian rejuvenation techniques. Therefore, from our point of view, the most appropriate term for these procedures is “ovarian activation techniques“, as we would increase the number of eggs, but not their quality.
Although a large number of procedures are being evaluated, following a scientific review of the available evidence, we have established, in our clinics, those that have demonstrated safety for the patient and show positive clinical results.
One of these is the administration of Platelet Rich Plasma (PRP) into the ovary, in which a small portion of the patient’s own blood rich in growth factors is injected.
The other is Ovarian Cortex Fragmentation and Autotransplantation (OFFA) which activates the ovary by mechanically “damaging” its structure and has allowed some women with early menopause to become pregnant.
After years of research, these techniques have proven to be safe and we know what the contraindications are. This is a necessary premise to be able to start their application.
However, although pregnancies and improvements in the number of eggs obtained have been reported, more studies are needed to prove that the treatment is responsible for the result. This means that the benefit of the procedure is not guaranteed; we do not have exact data on the percentage of effectiveness or on the type of patients who will respond best to the treatment.
Another aspect to keep in mind is that evidence from future studies may change the application protocols or the criteria for including or excluding patients for use.
Studies have evaluated these techniques in a varied group of patients: patients with low response, with suboptimal responses to stimulation, with early menopause and with physiological menopause over the age of 40.
However, so far, they have only shown improvement in certain patients with particular characteristics. It is therefore up to the medical team to assess whether the treatment can be effective in each specific case.
Low ovarian response is the collection of 3 or fewer eggs when we perform an ovarian stimulation treatment. We can predict this low response when ovarian reserve markers are decreased.
Research is continuously focused on increasing this ovarian response, as the number of eggs is the most important factor for the success of IVF, especially if the quality is compromised.
Studies show that in these patients the administration of PRP (Platelet Rich Plasma) is the technique that has shown an improvement in ovarian response, and we are applying it in the stimulation protocols, along with other complementary treatments.
It’s a very simple procedure in which we process a sample of the patient’s own blood to obtain a platelet-rich portion that we administer into the ovary. The platelets release a large amount of growth factors that act on the organ where we apply them. The procedure is similar to that performed during ovarian puncture for egg retrieval.
At present, the available evidence does not recommend this treatment in patients who are already in menopause. We would therefore apply it to those patients in whom, despite there is a response to treatment, this response is low.
There’s no age limit for its application, but the treatment will not improve the prognosis in older patients as it does not affect the quality of the egg, so it is possible that the doctor may advise against its use, as is the case with in vitro fertilisation treatment itself.
There’re some medical contraindications to the use of PRP the doctor must study, although no side effects of the treatment have been reported according to the available data. The risks are those of the ovarian puncture itself, similar to egg retrieval. They are very rare and occur in less than 1 in 500 punctures. They may consist of slight bleeding or pain, and very rarely risk of infection or puncture of areas around the ovary.
When there’s a definitive depletion of the ovarian reserve, the probability of achieving pregnancy with one’s own eggs is practically nil and the indicated treatment is egg donation.
In some patients, the eggs’ loss or depletion occurs at an early age, finding themselves in menopause before the age of 40, a situation known as ovarian failure or early menopause. These patients may have some spontaneous cycles and pregnancies, but it’s not possible to predict their occurrence.
Ovarian fragmentation and autotransplantation (OFFA) is a technique with which spontaneous pregnancies and pregnancies after in vitro fertilisation have been reported in this type of patient.
It requires laparoscopy, surgery in which we introduce a camera and some instruments through small incisions in the abdomen. This allows us to visualise the abdominal cavity and remove part of the ovary, which is then fragmented into small cubes and reinserted. It has been shown that this “mechanical damage” caused to the ovary by fragmentation may activate a small pool of inactive eggs that exists in patients with early menopause.
Most of the positive results have been obtained in patients under the age of 36, and we will always perform it in patients under the age of 40. For the moment this treatment is not intended for patients with low ovarian reserve, in whom the ovary still responds to stimulation.
Laparoscopy is a routine technique performed by gynaecologists for multiple problems such as the removal of ovarian cysts. The risks would be those of any surgery of these characteristics, no added risk has been observed with fragmentation.
As in the case of PRP, there are a series of contraindications to be considered, such as the presence of ovarian pathology, the existence of a single ovary, or ovarian failure due to genetic causes or after chemotherapy.
No treatment can stop the gradual loss of eggs or improve egg quality, so in this case the indicated treatment would still be donation.
The use of new techniques in this group of patients should only be part of research studies, or after the existence of strong scientific evidence in favour of their use.
In recent years, the Low Ovarian Reserve Unit has experienced important advances that have allowed us to improve the prognosis in patients with low ovarian response.
Pharmacogenetics has allowed us to design a specific treatment for each patient, different stimulation strategies have been implemented, such as the accumulation of eggs in double stimulation or stimulations in different phases of the cycle. These new ovarian activation techniques are yet another attempt to recover the greatest number of eggs in patients or even to obtain an ovarian response in patients who had not previously had one. The objective will always be to try to achieve pregnancy with the patient’s own eggs as far as the available treatments allow. In some cases, the only reasonable option to achieve pregnancy will be egg donation.
The most important thing is to be guided by the professional, who must explain whether any of these new techniques is advisable and whether there may be a benefit, so as not to fall into treatments with uncertain or misleading results.
Thus, based on the available evidence, the doctor will be able to advise against one type of technique altogether, or not to recommend continuing with the assisted reproduction treatment.
Broadly speaking, they are different terms for the same substance. Platelet-rich plasma is a portion of the patient’s blood that has a higher concentration of platelets than the baseline concentration.
Platelets release growth factors, so increasing the number of platelets in the sample used would increase the concentration of growth factors released into the plasma. These growth factors are responsible for the beneficial effect on ovarian activation.
However, there’re different techniques and systems available to obtain the sample in the laboratory, and the method used can influence the final number of platelets contained in the sample and thus the concentration of growth factors released. A concentration of 1,000,000 platelets per µl has been considered the ideal value to ensure optimal growth factor delivery. Some commercially available kits ensure a known concentration of growth factors in advance, although it is up to the clinic’s laboratory to validate that their samples contain the appropriate concentration of platelets used in the studies available for intraovarian PRP.
Double IVF
Double IVF for low ovarian reserve
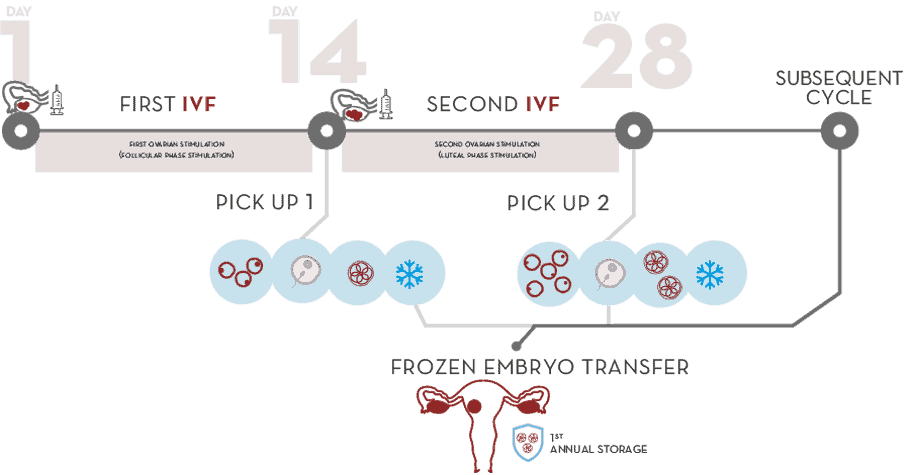
Two in vitro fertilization in one cycle: more embryos, more possibilities
Double IVF consists of performing a double in vitro fertilisation (IVF) in a single cycle, with the aim of adding to the first egg collection, that takes place in the first half of the cycle just before ovulation, a second one, and cryopreserving the embryos generated. We then start the second stimulation in the luteal phase (after ovulation) with a new egg collection, with the subsequent in vitro fertilisation and vitrification of the obtained embryos, adding them to the previous ones. This way we obtain a greater number of embryos than with conventional IVF.
The embryo transfer is carried out in a new cycle without the possible effects of an additional ovarian stimulation that could alter endometrial receptivity.
Double IVF for low ovarian reserve
Triple IVF
Some patients diagnosed with low ovarian reserve, a third stimulation with subsequent in vitro fertilisation may be indicated to increase the possibility of obtaining suitable embryos.
R&D&I: Evidence from successive double stimulation
The results of the research initiated in 2019 at Instituto Bernabeu for the treatment of patients with low ovarian response confirm the usefulness of consecutive ovarian stimulation protocols. This has led to an improvement in the overall results. This is indicated by research work such as that presented at the ESHRE 2021 Congress (European Society Human Reproduction & Embriology).
- Follicle-stimulating hormone receptor genotype and its influence on the results of double ovarian stimulation in IVF cycles
- And in ESHRE 2019, among others. The luteal phase of double ovarian stimulation treatment (DuoStim) provides higher oocyte and blastocyst yield in unselected infertile patients: a retrospective, same-patient, cohort study
Advantages
Emotional. This technique explores the possibilities of becoming a mother with your own eggs, avoiding resorting to egg donation. It reduces the waiting time and the treatment duration, which is concentrated in a single cycle.
Economic. Instituto Bernabeu’s priority is the pregnancy of its patients. A diagnosis of low ovarian reserve usually requires more complex and therefore more expensive treatments. In order to make them more accessible, we have created the double consecutive IVF, reducing a large part of the cost involved in carrying out several standard in vitro fertilisations.
Effective. The efficiency of the frozen embryo significantly exceeds that of the oocyte. Therefore, the chances of embryo nesting and the ongoing pregnancy rate are increased.
More natural transfer. Delayed embryo transfer allows us to use protocols that can improve the ovarian response without worrying about whether such stimulation could harm uterine receptivity. The transfer is carried out in a subsequent natural cycle or in which the uterus is specifically prepared to optimise its receptivity, thus increasing the chances of pregnancy.

LOW OVARIAN RESERVE RESEARCH
Advances in Low Reserve research
At Instituto Bernabeu, our Poor Responders Unit is a pioneer in this field of research. As a result of our commitment towards research, our institute was awarded by the American Society for Reproductive Medicine (ASRM) in 2012 for a paper on genetic polymorphisms in Poor Responders. Further to the above, we have been the first clinic worldwide to develop a pharmacogenetics concept applied to ovarian stimulation by introducing out new IBgenIVF test.
Currently, our main research areas are focused in three main aspects:
- Genetic factors that cause ovarian aging with the purpose of developing predictors to assist women when planning their reproductive life.
- Pharmacogenetic advances that will allow us to customise our stimulation protocols depending on each patient’s genetic profile, thus improving their response to hormone application.
- Exploring new forms of stimulation through clinical trials in low responders, such as new luteal phase research studies.
- Administer the patient’s own platelet-rich plasma (PRP) to the ovary to favour the activation of “sleeping follicles” and increase the number eggs.
- To perform new ovarian activation techniques for patients in early menopause, such as ovarian cortex fragmentation and autologous transplantation (OFFA).
Encouraging results are being achieved in many patients who would otherwise need to turn to egg donation.

Our high level of specialisation in poor responder patients allows you to have access to all specialised practitioners required to carry out a personal study plan during your appointment, to ensure that you can complete all the required diagnostic test to analyse and design your customised treatment plan in just one day.
Female partner
- Poor response risk based on your own genetic profile. IBgen IVF.
- Anti-Müllerian hormone.
- Karyotype.
- Fragile X.
- High resolution ultrasound
- Personalized analysis of your medical history
- Assessment consultation by a low ovarian reserve specialist.
- Followed by a new specialist consultation in order to assess and design your own treatment plan (may be done by videoconference).
