What is a biochemical pregnancy or miscarriage?
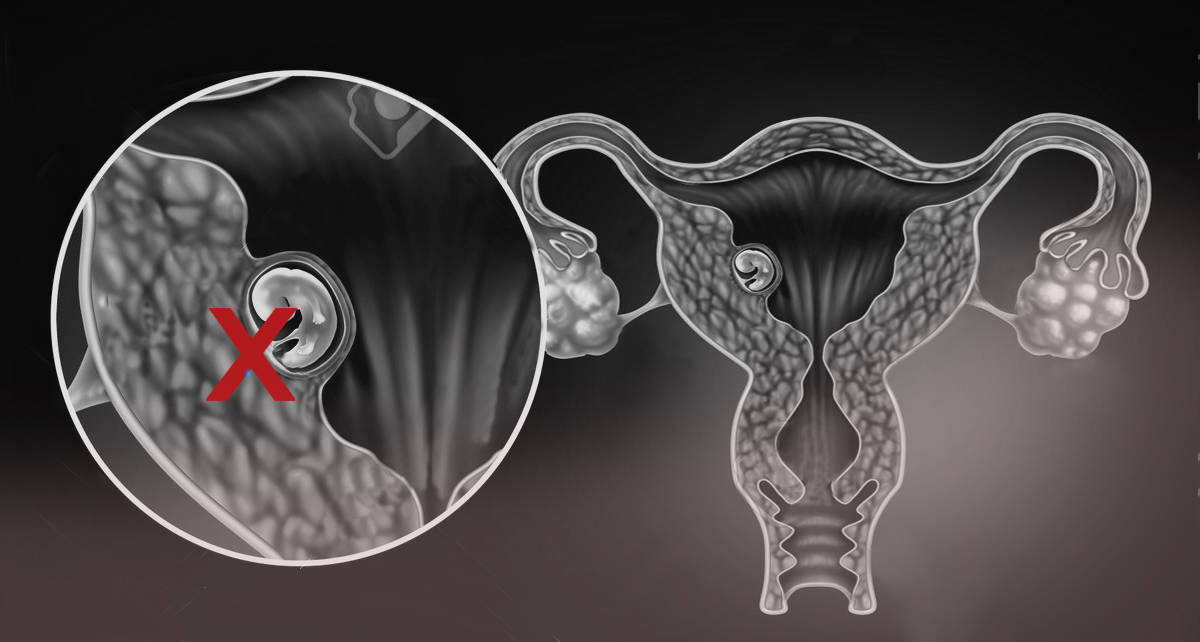
Biochemical pregnancy or miscarriage occurs when an embryo, which initially implants in the uterus, stops developing. The pregnancy test is positive but the HCG hormone subsequently decreases until it becomes negative a few days later with the onset of menstruation.
‘Biochemical pregnancies’ are not exclusive to assisted reproduction treatments and also occur in natural pregnancies. Most of them go undiagnosed because they are mistaken for a delay in menstruation.
Índice
What is the incidence?
Biochemical pregnancy has an incidence of 13-22%, not varying whether fresh or vitrified embryos are transferred. The incidence is similar to that of the general population who do not undergo in vitro fertilisation.
Does biochemical pregnancy hinder the possibility of a future pregnancy?
A positive pregnancy test is the result of uterine implantation, so a biochemical pregnancy indicates that the endometrium has been receptive to the embryo. Just as there are embryos that are incapable of implanting, others manage to do so, but have insufficient potential to achieve a clinical and evolutionary pregnancy. Cases of repeated biochemicals miscarriages are rare.
Most common causes?
Knowledge about biochemical pregnancies in IVF cycles remains limited and the existing literature on associated factors often presents conflicting data.
While embryonic chromosomal alterations have been proposed as a possible cause, more recent studies have shown that biochemical pregnancy rates are not affected even when euploid embryos are transferred in PGT-A cycles.
Other factors that do not seem to be associated with an increased risk of biochemical pregnancies are: maternal age, body mass index (BMI), ovarian reserve, embryos from own and donated oocytes in PGT-A cycles, ICSI or IVF technique and antiphospholipid antibody positivity.
Factors that may increase the risk of biochemical pregnancies appear to be polycystic ovarian syndrome, poor embryo quality, reduced endometrial thickness, sperm DNA fragmentation and progesterone deficiency.rns that these patients may have, and give them all the necessary information that they need to overcome the situation and continue to try and reach their goal.
Dr. Rosa Maria Daurelio (num. 282865587), Gynecologist and Reproductive Medicine Specialist at Instituto Bernabeu
IT MAY ALSO BE OF INTEREST TO YOU:
- Implantation failure and recurrent miscarriage Unit in Instituto Bernabeu
- Molar pregnancy or hydatidiform mole
- Ectopic pregnancy
- Anembryonic gestation
- Pregnancy check-ups and labour
